Friday, June 29, 2007


Multiple Myeloma
- Clinical
- Average age is 60-70
- Men much more common than women
- Most have an elevated serum protein with 80-90% in the globulin fraction, especially IgG
- Bence-Jones protein in 40-60% of patients (light chains)
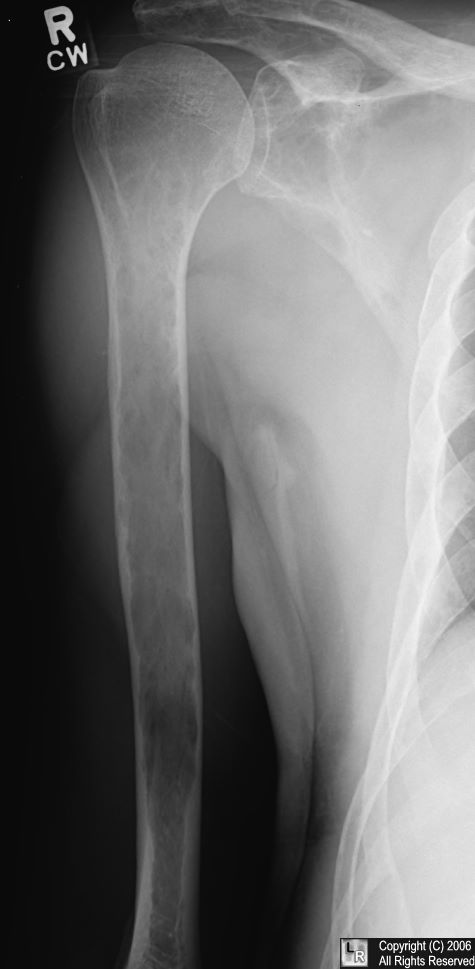
- X-ray findings
- Osteoporosis is most common skeletal abnormality in this disease
- Lesions are usually multiple and found in vertebrae, ribs, skull, pelvis, and femur
- Over 50% of solitary lesions are found in vertebrae
- Mandible involved in 1/3 of patients with diffuse involvement
- Widespread lucencies in bone
- Discrete, “punched-out” lesions
- Uniform in size
- Distinctive to MM are the lucent, elliptical, subcortical shadows, especially in long bones=endosteal scalloping
- Due to buttressing since MM is usually a slower process than mets
- In spine, MM destroys body and spares pedicle
- DDX: mets and disuse osteoporosis
- MM is more widespread
- More discrete holes in MM
- Large foci of coalescence more often due to mets
- Severe disuse osteoporosis may simulate bone changes of MM
- Sclerosis is usually seen only with treatment or fracture
- Bone scans may typically be negative and many hot areas on scan may be healing fractures
- Most believe that almost all patients with a solitary plasmacytoma will develop multiple myeloma
- Solitary plasmacytoma produces “soap-bubbly” expansile, septated lesion, when characteristic

Ductography
 | What is Galactography?Galactography, or ductography, is a mammographic technique that involves injection of a contrast agent (dye) into a milk duct. This study may be useful in the evaluation of unilateral spontaneous nipple discharge that is bloody. (Nipple discharge that is milky, yellow, or green is rarely associated with breast cancers.)
What can I expect from the examination?The initial radiologic evaluation of nipple discharge includes a mammogram. If no abnormality is visible, a galactogram may be indicated. The duct must be discharging on the day of the study in order to identify the correct orifice to be cannulated. A tiny blunt-tipped catheter (called a cannula) is inserted into the discharging duct and a small (approximately 1 ml) amount of contrast agent is injected. Additional mammographic images are obtained. Some patients report a sensation of "fullness" during the examination, but no sharp pain or burning should be experienced. If an abnormality is detected on the galactogram, surgical excision is recommended.The most common cause of abnormal nipple discharge is a papilloma (a benign tumor that grows from the wall of a duct). Fewer than 10% of patients with abnormal duct discharge have a related breast malignancy. |
The figure to the left is a galactogram. Note that the contrast material dramatically increases the visibility of the ducts. |
Wednesday, June 20, 2007

Medical Centers near The Belamar
| Medical Centers near The Belamar. |  | |||||||||
|

Technical Standards

 The College of Medicine’s goal is the broad preparation of students to practice medicine. Regardless of eventual specialty selection, students must demonstrate competence in those intellectual, physical, and social tasks that together represent the fundamentals of medical practice. Applicants and students will be judged not only on their scholastic achievement and ability,but also on their intellectual, physical, and emotional capacities to meet the full requirements of the school’s curriculum. As an advisory committee to the Dean, the Admissions Committee is instructed to exercise judgment on behalf of the faculty members to recommend the entering class, and to consider character, extracurricular achievement, and overall suitability for the medical profession on the basis of information in the application, letters of recommendation, and personal interviews.
The College of Medicine’s goal is the broad preparation of students to practice medicine. Regardless of eventual specialty selection, students must demonstrate competence in those intellectual, physical, and social tasks that together represent the fundamentals of medical practice. Applicants and students will be judged not only on their scholastic achievement and ability,but also on their intellectual, physical, and emotional capacities to meet the full requirements of the school’s curriculum. As an advisory committee to the Dean, the Admissions Committee is instructed to exercise judgment on behalf of the faculty members to recommend the entering class, and to consider character, extracurricular achievement, and overall suitability for the medical profession on the basis of information in the application, letters of recommendation, and personal interviews.The Liaison Committee on Medical Education, which accredits the Medical School, requires that the curriculum provide a general professional education that will enable each student to pursue graduate training in a variety of disciplines. Meeting this requirement necessitates that the curriculum assists students in developing broad knowledge, skills, and behaviors; enabling ongoing self-directed learning
and further training; and preparing them to deliver competent medical care. The basic sciences curriculum includes the study of anatomy, biochemistry, histology, pathology, and pharmacology and is designed to establish a core of knowledge necessary for clinical training. The clinical curriculum includes diverse experiences in primary care, family medicine, internal medicine, obstetrics and gynecology, pediatrics, psychiatry,
surgery, diagnostic imaging, pathology, emergency medicine, and geriatrics, in both ambulatory and inpatient settings. These rotations develop the ability to practice medicine independently, regardless of the future choice of specialty. To graduate, each
student is required to pass each required course and clinical rotation.

The following technical standards specify those attributes that the faculty members consider necessary for completing medical school training; successful completion of these requirements will enable each graduate to subsequently enter residency and clinical practice. These standards describe the essential functions that students must demonstrate if they are to fulfill the requirements of a general medical education.
Thus, these standards constitute prerequisites for entrance into, continuation in, and graduation from medical school. The University of Kentucky College of Medicine will consider for admission to the medical school any applicant who demonstrates the ability to perform or to learn to perform the skills listed in this document. Applicants are not required to disclose the nature of any disability to the Admissions Committee; however, any applicant with questions about these technical requirements is strongly encouraged to discuss the issue with the Assistant Dean for Admissions before beginning the interview process. If appropriate, and upon the request of the applicant or student, reasonable accommodations may be provided. Certain chronic or recurring illnesses and problems that interfere with patient care or safety may be incompatible with medical training or practice. Deficiencies in knowledge base, judgment, integrity, character, or professional attitude or demeanor that may jeopardize patient care may be grounds for failure of a course or a rotation and possibly for dismissal. A student must possess aptitude, abilities, and skills in five areas: Observation, Communication, Sensory and Motor Coordination or Function, Intellectural-Conceptual Integrative and Quantitative Abilities and Behavioral Attributes. Back to Top

Students must be able to observe demonstrations and to conduct experiments in the basic sciences, including but not limited to physiologic and pharmacologic demonstrations in animals, microbiologic cultures, and microscopic studies of microorganisms and tissues in normal and pathologic states. A student must be able to observe a patient accurately at a distance and close at hand, noting nonverbal and verbal signals.  Specific vision-related requirements include but are not limited to the
Specific vision-related requirements include but are not limited to the
following abilities: skin, culture media, and dipstick tests; visualizing and discriminating findings on x-rays and other imaging tests; reading written and illustrated material; observing demonstrations in the classroom, including projected slides and overheads; observing and differentiating changes in body movement; observing anatomic structures; discriminating numbers and patterns associated with diagnostic instruments and tests, such as sphygmomanometers and electrocardiograms; and using instruments competently, such as stethoscope, otoscope, ophthalmoscope, and microscope.

changes in mood, activity, and posture; and perceiving verbal and nonverbal communication. Communication includes not only speech but also listening, reading, and writing. Medical education presents exceptional challenges in the volume and breadth of required reading and the necessity of imparting information to others. Students must be able to communicate quickly, effectively, and efficiently in oral and written English with all members of the health care team. Specific requirements include but are not limited to the following abilities: communicating rapidly and clearly with the medical team on rounds; eliciting a thorough history from patients; and communicating complex findings in appropriate terms to patients and to various members of the health care team (fellow students, physicians, nurses, aides, therapists, social workers, and others). Students must learn to recognize and promptly respond to emotional communications such
as sadness, worry, agitation, and lack of comprehension of physician communication. Each student must be able to read and to record observations and plans legibly, efficiently, and accurately in documents such as the patient’s record. Students must be able to prepare and communicate concise but complete summaries of individual encounters and complex, prolonged encounters, including hospitalizations. Students must be able to complete forms according to directions in a complete and timely fashion.

Medical Physics Group
About Us
The Medical Physics Group is primarily based at the Radiation Oncology Department, Newcastle Mater Hospital (NMH) and have conjoint appointments with the University of Newcastle. The group is concerned with the physics that underlies the practice of radiation therapy for the treatment of cancer and have a strong track record in dosimetry research. Our research interests fall into the following broad topic ranges (see individual pages for more details):
- Quality assurance and dosimetric verification, particularly for clinical trials
- Imaging and treatment localization
- Dosimetry with amorphous silicon electronic portal imaging devices
- Intensity modulated brachytherapy
- Dosimetric verification of brachytherapy
We also have active clinical treatment and development programs including IMRT, HDR brachytherapy, MRI and PET in treatment planning, and fiducial marker guided prostate treatment.
Enquiries from prospective students are welcome. Please contact Peter Greer or Martin Ebert